The Visual Guide to
Bovine Reproduction
- Uterine Torsion
- Strangulated Umbilical Cord
- Pelvic Subluxation
- Prolapsed Vagina
- Prolapse of the Bladder
- Ruptured Prepubic Tendon
- Prolonged Gestation
- Hydrops Allantois
- Hydrops Amnii
- Mummification
- Maceration
Accidents of Gestation: Prolapsed Vagina
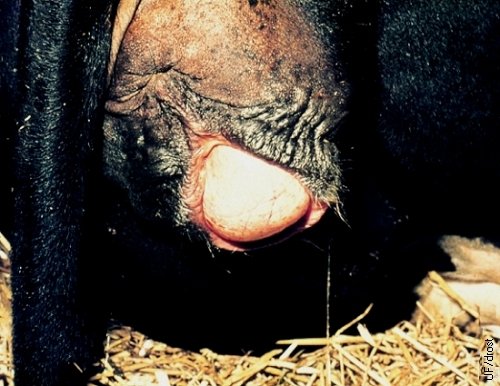
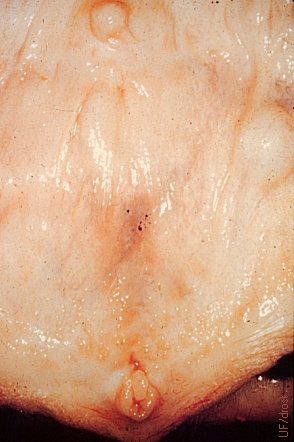
Early Prolapsed Vagina.
In the early stages of an incipient vaginal prolapse, the hyperemic mass will only present itself in the recumbent cow, and is pulled forward and back inside as she rises. Exposure of the mucosa to the air progressively leads to drying, irritation, swelling, inflammation, pain, straining, causing the prolapsed mass to enlarge so it can no longer go back inside.
Roberts SJ (1973)
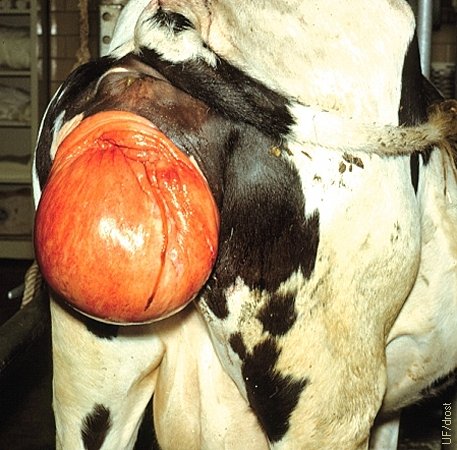
Extensive Vaginal Prolapse.
This prolapsed mass was thoroughly cleaned up for the picture. Manure and bedding typically cling to the sticky mucous membrane of the exposed vagina. Trauma is common
Roberts SJ (1973)

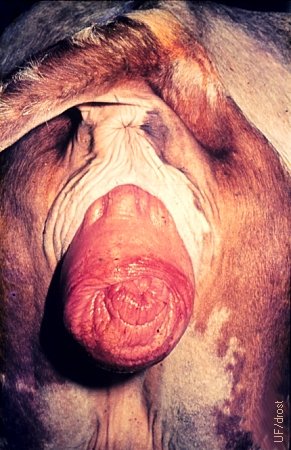
Cervicovaginal Prolapse.
This lateral view illustrates a typical cervicovaginal prolapse in a nonpregnant cow.
Utrecht (1976)
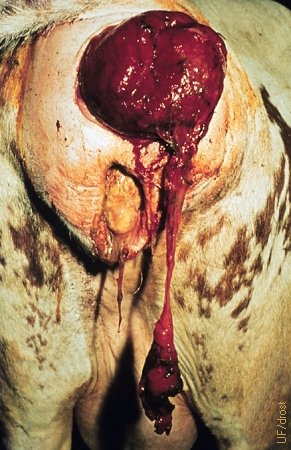
Cervicovaginal Prolapse.
Posterior view of a cervicovaginal prolapse in a nonpregnant cow.
Utrecht (1976)

Cervicovaginal Prolapse in a Braford Cow.
Braford cow with a recurring prolapse of her cervix and vagina.
Kelleman AA (2011)

Cervicovaginal Prolapse Close Up.
The prolapsed cervix and vagina of this Braford cow are considerably traumatized, swollen, indurated, and contaminated. They had been out for several days.
Kelleman AA (2011)

Cervicovaginal Prolapse Close Up.
Braford cow with a recurring prolapse of her cervix and vagina. Indurated mass of several days duration.
Kelleman AA (2011)

Cervicovaginal Prolapse Close Up.
Traumatized indurated mass of several days duration.
Kelleman AA (2011)

Contaminated Cervicovaginal Prolapse.
Severely contaminated and swollen cervico-vaginal mass of several days duration.
Kelleman AA (2011)

Cleaning of the Cervicovaginal Prolapse.
Clean up of a severely contaminated and swollen cervico-vaginal mass, under epidural anesthesia.
Kelleman AA (2011)

Cervicovaginal Prolapse Replacement.
After clean up the swollen mass is wrapped tightly to reduced the edema prior to replacement.
Kelleman AA (2011)

Cervicovaginal Prolapse Replacement.
After cleaning and compressing the mass it is ready for reinsertion into the vagina.
Kelleman AA (2011)

Cervicovaginal Prolapse Replacement.
The clean, disinfected, still edematous mass is returned to the vagina, under epidural anesthesia.
Kelleman AA (2011)

Cervicovaginal Prolapse Replacement.
The clean, disinfected, still swollen mass is gently returned to the vagina, under epidural anesthesia.
Kelleman AA (2011)

Cervicovaginal Prolapse Replacement.
The clean, disinfected, still swollen mass is gently returned to the vagina, under epidural anesthesia.
Kelleman AA (2011)

Cervicovaginal Prolapse Replacement.
The prolapsed mass is advanced into the anterior vagina.
Kelleman AA (2011)

Cervicovaginal Prolapse Replacement.
The prolapsed cervix and vagina have been replaced under epidural anesthesia.
Kelleman AA (2011)

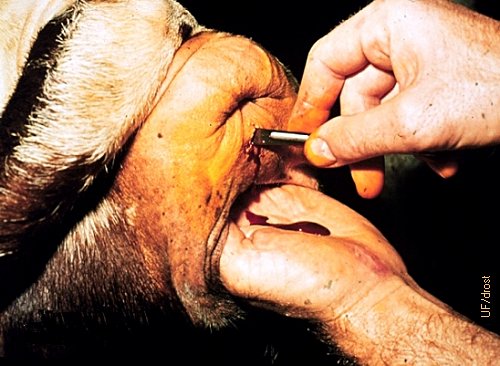
Cervicovaginal Prolapse Retention.
The finger points at the location of the dorsal commissure of the vulva.
Kelleman AA (2011)

Cervicovaginal Prolapse Retention.
The four circles indicate the locations of the placement of the retention suture pattern at the hairline just lateral to the vulvar lips.
Kelleman AA (2011)

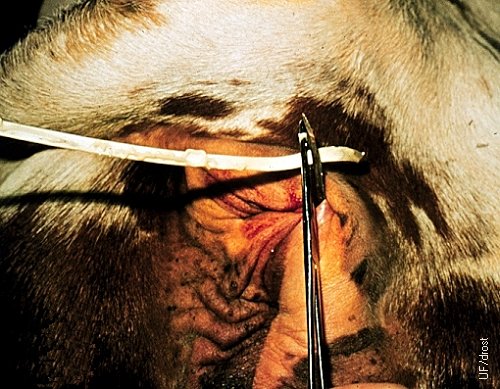
Cervicovaginal Prolapse Retention.
15 cm needle with curved cutting tip for placement of the umbilical tape for the internal cruciate suture pattern.
Kelleman AA (2011)

Cervicovaginal Prolapse Retention.
Initial insertion of the needle at left lower circle in the direction of the right upper circle [for a left handed surgeon].
Kelleman AA (2011)

Cervicovaginal Prolapse Retention.
The needle exited at the upper right circle and will next be inserted from the left upper circle to the right lower circle, completing the pattern, of a cross stitch on the inside and two parallel horizontal bars on the outside.
Kelleman AA (2011)

Cervicovaginal Prolapse Retention.
Left upper insertion to right lower exit, to complete the pattern.
Kelleman AA (2011)

Cervicovaginal Prolapse Retention.
Each cross over of the needle is in two steps, from the skin to the inside of the labia, and vice versa. Shown is the last of four bites.
Kelleman AA (2011)

Cervicovaginal Prolapse Retention.
The needle emerges from the final hole at the lower right, after the fourth bite.
Kelleman AA (2011)

Cervicovaginal Prolapse Retention.
Tightening the suture prior to tying the knot.
Kelleman AA (2011)

Cervicovaginal Prolapse Retention.
Tying the knot of the internal cruciate pattern.
Kelleman AA (2007)

Cervicovaginal Prolapse Retention.
Inserting a finger to test the patency of the vestibule for urination prior to tying the final knot.
Kelleman AA (2011)

Cervicovaginal Prolapse Retention.
Final closure. The sutures are easy to remove by cutting the horizontal sutures when the cow goes into labor.
Kelleman AA (2011)

Cervicovaginal Prolapse Retention.
A Buehner needle can alternatively be used to place the internal cruciate suture pattern.
Kelleman AA (2011)

Restraint in the Chute.
Braford cow restrained in the chute for correction of a vaginal prolapse. Cervico-vaginal prolapses tend to be more prevalent in Brahman and Hereford breeds and their crosses.
Kelleman AA (2011)

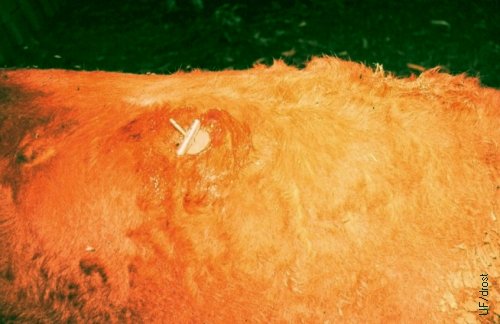
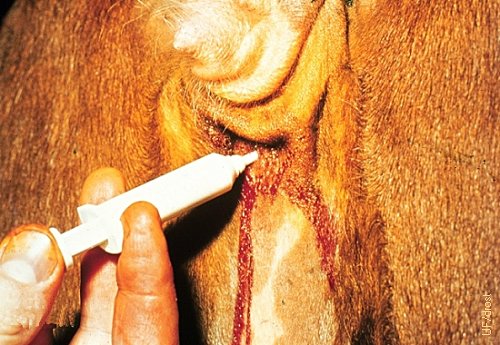
Epidural Anesthesia.
Placement of the needle in the center of the first intercoccygeal space at a right angle to the normal contour of the tailhead. Injection of 2% Lidocaine.
Drost M (2011)

Retention Suture Pattern 1.
An internal cruciate stitch is placed after replacement of the vaginal prolapse under epidural anesthesia. The orange circles identify the entry and exit sites of the needle.
Drost M (2011)

Retention Suture Pattern 2.
Close up of the location of the four entry and exit sites of the needle at the junction of the vulvar lips and the skin [at the hair line for greatest strength]. Pattern for a left handed surgeon: lower left to upper right, then upper left to lower right; for a right handed surgeon: lower right to upper left, the upper right to lower left.
Drost M (2011)

Retention Suture Pattern 3.
Fifteen centimeter straight needle with a curved cutting point and double threaded with umbilical tape.
Drost M (2011)

Retention Suture Pattern 4.
The needle entered from the lower left circle and was aimed at the upper right circle. The first bite is from the left hairline through the left labia.
Drost M (2011)

Retention Suture Pattern 5.
Second bite of the needle from the inside of the right labia directed to the right upper exit point.
Drost M (2011)

Retention Suture Pattern 6.
The tape next goes externally, and horizontally from the right upper exit point to the left upper entry point.
Drost M (2011)

Retention Suture Pattern 7.
The tape has entered at the upper left through the left labia, and is now directed to the right lower exit point of the right labia.
Drost M (2011)

Retention Suture Pattern 8.
Fourth bite exited through the right labia at the lower left. The tape is ready to be tied horizontally and externally to complete the pattern.

Failure to Remove the Retention Suture.
Angus cow during late gestation with a fresh cervico-vaginal prolapse. Some mucus is dripping from underneath the prolapsed mass.
Lane VM (2013)

Failure to Remove the Retention Suture.
As the cow went into labor the owner failed to remove the retention suture. The cow forced the calf through the weakened vaginal wall and through the perineal skin. Unattended, unassisted spontaneous vagina delivery. Picture was taken several hours after delivery when the traumatized, necrotizing vagina wall had dried out.
Lane VM (2013)

Failure to Remove the Retention Suture.
The traumatized necrotic prolapsed vagina has been replaced via the large tear in the perineal skin.
Lane VM (2013)

Cervical Prolapse.
Flaccid, enlarged hyperemic cervical folds have prolapsed. Induration and swelling due to inflammation and contamination have not yet occurred.
El Naggar MA (2005)

Prolapse of the Cervix.
The enlarged hyperemic cervix can prolapse when poor vestibular tone and abdominal pressure are present, and the cow lies down.
El Naggar MA (2005)

Prolapse of the Cervix.
The enlarged hyperemic cervix can prolapse when poor vestibular tone and abdominal pressure are present and as the cow lies down. This cow had a double cervical os.
Zawisza D (2012)

Prolapsed Rectum.
A prolapsed rectum is sometimes confused with a prolapsed vagina by the inexperienced observer, especially when the prolapsed mass is very dirty.
Drost M (1978)
Prolapsed Rectum.
Prolapsed rectum, not to be confused with prolapsed vagina, though often mistaken for the other by the inexperienced observer.
Utrecht (1976)

Rectal Prolapse.
Rectal prolapse in a beef heifer. This must not be mistaken for a vaginal prolapse.
Drost M (1978)

Rectal Prolapse.
Holstein cow with vaginal and rectal prolapses. Persistent forceful straining sometimes leads to prolapse of the rectum in addition to prolpase of the vagina.
Galvão K (2013)

Rectal and Vaginal Prolapse.
Chronic indurated vaginal prolapse and a concurrent indurated rectal prolpase.
Villarroel A (2013)

Prolapse of the Bladder.
Fortunately, prolapse of the bladder is a rare occurrence. It must differentiated from prolapse of the vagina and prolapse of the rectum, by anatomical landmarks.
Utrecht (1976)
Cystic Vestibular Gland - Small.
The duct of the right vestibular gland (Bartholin gland) has become occluded, leading to accumulation and distention. Vestibular glands are the homologues of the bulbo-urethral glands in the male. Slight enlargement goes unnoticed. If distension becomes large enough, the bulging mass will part the lips of the vulva and resemble a beginning prolapse of the vagina.
Roberts SJ (1973)

Cystic Vestibular Gland Greatly Distended.
The duct of the right vestibular gland (Bartholin gland) has become occluded leading to accumulation and distention. Here the distention is large enough to part the lips of the vulva, and the mass may be mistaken for an early prolapse of the vagina. Treatment of this infrequently occurring malady is by incision and drainage. Vestibular glands are the homologues of the bulbo-urethral glands in the male.
Roberts SJ (1973)

Vaginal Prolapse Repair with Loops of Tape
Retention of the prolapsed vagina by means of the bilateral placement of four loops of tape in the hairline followed by a bootlace pattern using umbilical tape. This allows ready removal of the retention "suture" when the cow goes into labor.
Drost M (1978)

Instruments and Devices for Vaginal Prolapse Repair.
Various instruments and retention devices for correction of a vaginal prolapse. At the top is a Buehner needle and a coil of braided Buehner tape for the placement of a purse string suture (used only when the cow is not pregnant because removal is difficult); toggle devices are used in sets of three or four; hog rings are used bilaterally for a bootlace pattern; the dark red device is a U-saver, a retention device for vaginal prolapse in ewes [the center paddle portion is inserted vertically, then turned 90 degrees, after which the two ends are tied to the wool].
Drost M (1978)

Instruments for Repair of a Prolapsed Vagina.
The top three devices are toggle bolts and require a detachable sharp needle for placement at the hair line. Direct placement of horizontal mattress sutures requires the use of stents to prevent the heavy suture material from cutting through. Hog rings can be placed bilaterally at the hair line with the applicator to serve as rings for a shoe lace pattern. Generally, three or four retention sutures or "bars" are placed loosely enough to permit urination. These are all readily removable retention devices for when the cow goes into labor.
Drost M (1978)

Retention with Prolapse Pins.
Retention of the prolapsed vagina by means of prolapse pins inserted at the hairline. The little wooden spheres can readily be removed when the cow goes into labor.
El Naggar MA (2005)

Vaginal Prolapse Repair with Hog Rings.
Retention of the prolapsed vagina by means of the bilateral placement of four hog rings at the hairline followed by a bootlace pattern using umbilical tape. This allows ready removal of the retention tape when the cow goes into labor.
Drost M (1978)

Prolapsed Vagina in a Nonpregnant Cow.
Prolapse of the vagina occurs most commonly in the late pregnant animal. If it occurs in the nonpregnant individual it may be corrected with the use of a purse string pattern, like the Buhner pattern, which is contraindicated in the pregnant cow because it is difficult to remove. [size of the square tile is 15 cm].
Roberts SJ (1973)

Repair of Prolapsed Vagina in the Nonpregnant Cow.
Instruments needed for the placement of a deep purse string suture with the Buehner needle and woven Buehner tape.
Drost M (1978)

Purse String Suture in Place.
Correction / retention of the prolapsed vagina with a purse string suture. Enough diameter / lumen must be left for the cow to urinate.
Drost M (1978)

Minchnev Technique for a Prolapsed Vagina.
The finger points at the site where the needle will exit after it is pushed up from inside of the vagina. The objective of this technique is to anchor the roof of the vagina bilaterally and permanently to the sacrosciatic ligament. Commercially available devices, known as Johnson buttons are placed in the same location and consists of two 7 cm discs and a shaft. The shaft with one disc attached is pushed up from within the vagina, after which the second disc is placed externally like a washer on the shaft. The second disk is kept in place with a cotter pin.
Drost M (1978)
Minchnev Technique for a Prolapsed Vagina.
The principle of the Minchnev technique is to anchor the roof of the vagina bilaterally and permanently to the sacrosciatic ligament. In this illustration a shaft with a toggle bolt and washer is used. Commercially available devices, known as Johnson buttons are placed in the same location and consists of two 7 cm discs and a shaft. The shaft with one disc at the end is pushed up from within the vagina, after which the second disc is placed externally like a washer on the shaft. The second disk is kept in place with a cotter pin.
Drost M (1978)

Epidural Anesthesia.
Five cc of a 2% solution of Lidocaine is injected in the space between the sacrum and the first coccygeal vertebra, or between the first two coccygeal vertebrae.
Utrecht (1976)

Instruments for the Buehner Procedure.
Large Buehner needle and surgical instruments for the placement of a deep purse string suture to retain a prolapsed vagina in a nonpregnant cow. The white circle is a coiled piece of braided tape. The mastitis syringe is for medication of the tape and for injection into the two stab incisions upon completion of the procedure.
Utrecht (1976)

Cow after Replacement of the Prolapsed Vagina.
Cow restrained in stocks. The prolapsed vagina has been replaced under epidural anesthesia. She is ready for the placement of a retention suture.
Utrecht (1976)
Retention of the Prolapsed Vagina 1.
A stab incision is made in the perineum, through the skin halfway between the anus and the dorsal commissure of the vulva.
Utrecht (1976)

Retention of the Prolapsed Vagina 2.
A ventral stab incision is made through the skin just below the tip of the vulva.
Utrecht (1976)

Retention of the Prolapsed Vagina 2.
A ventral stab incision is made through the skin just below the tip of the vulva.
Utrecht (1976)

Retention of the Prolapsed Vagina 3.
Mastitis ointment is applied to medicate the braided tape.
Utrecht (1976)

Retention of the Prolapsed Vagina 4.
Insertion of the needle is started at 6 o'clock below the ventral commissure of the vulva. The needle is then directed deeply in a wide (up to the hairline) counterclockwise semicircle.
Utrecht (1976)

Retention of the Prolapsed Vagina 5.
The semicircle is completed at 12 o'clock where the tip of the needle exits via the dorsal stab incision.
Utrecht (1976)

Retention of the Prolapsed Vagina 6.
The trajectory of the straight needle is actually that of a semicircle.
Utrecht (1976)
Retention of the Prolapsed Vagina 7.
The tip of the Buehner needle, which has an eye, is threaded with the medicated tape.
Utrecht (1976)

Retention of the Prolapsed Vagina 8.
The tape is pulled through from top to bottom on the right side.
Utrecht (1976)

Retention of the Prolapsed Vagina 9.
The opposite semicircle is completed in the same manner, from 6 o'clock to 12 o'clock.
Utrecht (1976)

Retention of the Prolapsed Vagina 10.
The lead end of the tape is now threaded and subsequently pulled through its semicircle.
Utrecht (1976)

Retention of the Prolapsed Vagina 11.
he purse string is ready to be tightened by pulling down on both ventral ends.
Utrecht (1976)

Retention of the Prolapsed Vagina 12.
During tightening of the purse string two or three fingers are placed in the vulva to maintain enough room for urination.
Utrecht (1976)

Retention of the Prolapsed Vagina 14.
The knot is tucked in with a pair of forceps.
Utrecht (1976)
Retention of the Prolapsed Vagina 15.
Mastitis ointment is instilled in the ventral stab incision upon completion of the procedure.
Utrecht (1976)

Retention of the Prolapsed Vagina 16.
Mastitis ointment is instilled in the upper stab incision upon completion of the procedure, as well.
Utrecht (1976)

Cervico Vaginal Prolapse Repair 1.
After replacement of the prolapsed cervix and vaginal, under epidural anesthesia, a 1 cm skin incision is made along the midline halfway between the anus and the dorsal commissure of the vulva, and a second 1 cm incision below the ventral commissure. Here the Buehner needle is inserted into the ventral incision.
Drost M (2011)

Cervico Vaginal Prolapse Repair 2.
The tip of the Buehner needle has followed a semicircular trajectory from 6 o'clock via 3 o'clock to 12 o' clock, where it exits. Tape is inserted in the eye of the tip of the needle and is withdrawn through the trajectory.
Drost M (2011)

Cervico Vaginal Prolapse Repair 3.
While the tape is held, the tip of the needle is re-inserted at 6 o'clock to follow a semicircle via 9 o'clock to 12 o'clock, where it exits (again).
Drost M (2011)

Cervico Vaginal Prolapse Repair 4.
After the semicircle to the left, the tip of the needle exits the 1 cm incision in the perineum, where it will be threaded with the tape.
Drost M (2011)

Cervico Vaginal Prolapse Repair 5.
The tip of the needle is ready to be threaded with the tape.
Drost M (2011)

Cervico Vaginal Prolapse Repair 6.
The tip of the needle is threaded with the tape after which it is withdrawn through the semicircular trajectory to the left.
Drost M (2011)

Cervico Vaginal Prolapse Repair 7.
The threaded needle is withdrawn through the semicircular trajectory to the left.
Drost M (2011)

Cervico Vaginal Prolapse Repair 8.
The purse string suture is tied while two fingers are inserted in the vestibule to make sure there is sufficient room for urination.
Drost M (2011)


