
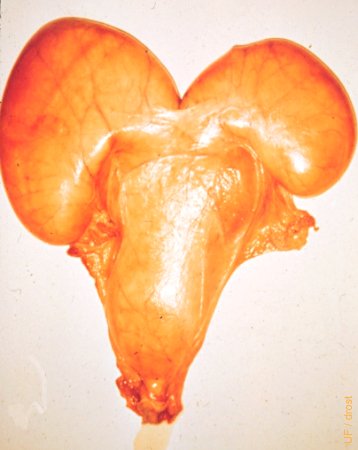
Normal Mare Tract.
Normal complete reproductive tract of a mare, plus the urinary bladder.
Drost M (1983)

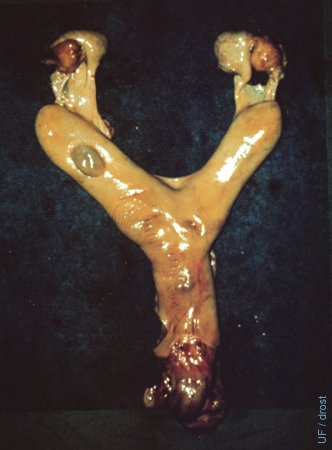
Normal Uterus.
This fresh specimen illustrates the anatomy of the adult equine uterus. The uterus is suspended by the broad ligament which is attached to the dorsal aspect of the uterus. The uterus is roughly T-shaped.
Drost M (1983)
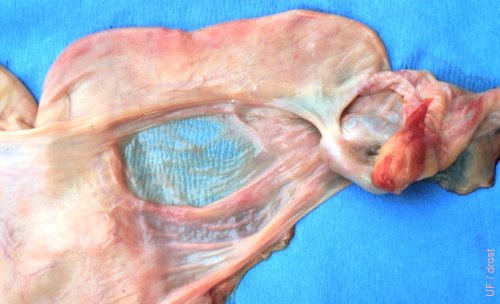
Broad Ligament.
Dorsal attachment of the broad ligament to the uterus.
Drost M (1983)

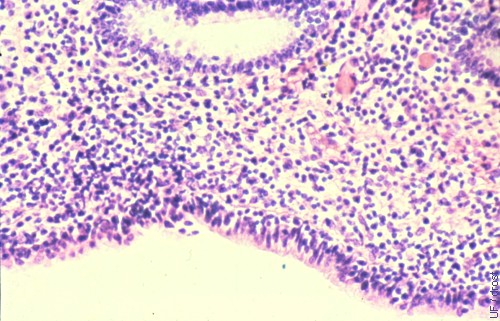
Metestrous Uterus.
Normal metestrous uterus. Complete reproductive tract.
McEntee K (1972)
Dilated Lymphatic.
Dilated lymphatic on the perimetrium of the left horn. No clinical significance in terms of fertility. It may be confusing to the palpater or on ultrasound examination.
Utrecht (1975)

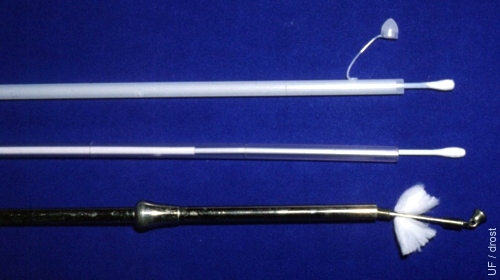
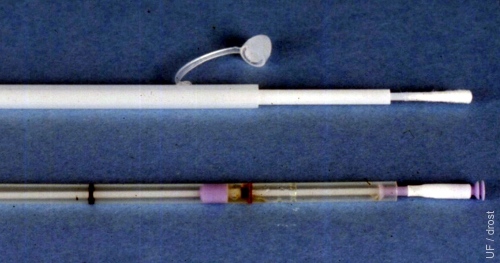
Uterine Culture Instruments 1.
Shown are, the Kalayjian culture instrument at the top, the unguarded swab in the middle, and the metal Knudsen instrument. Both the Kalayjian and the Knudsen are designed to protect the swab as it is passed through the vagina and cervix hence providing the opportunity to secure a true culture of the uterine lumen.
Asbury AC (1993)
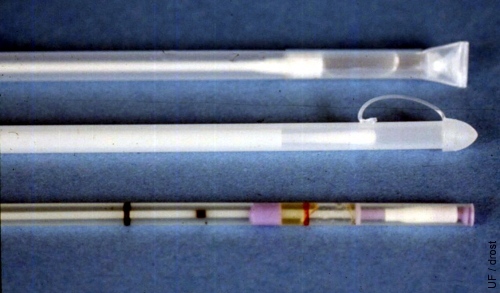
Uterine Culture Instruments 2.
Same instruments as in Uterine Culture Instruments 1, but with the swabs uncovered. The Kalayjian swab is protected by a plastic cap, attached to the casing. This cap can be used to obtain a scraping of the endometrium suitable for staining.
Asbury AC (1993)
Uterine Culture Instruments 3.
Guarded instruments. From top to bottom, the plain swab, the Kalayjian, and the Acu-CulShure culture instruments.
Asbury AC (1993)
Uterine Culture Instruments 4.
The swabs of the Kalayjian culture instrument at the top of the image, and the Acu-CulShure culture instrument have been pushed forward (exposed).
Asbury AC (1993)
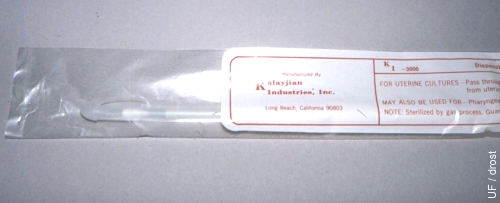
Kalayjian Culture Instrument.
Close-up of the tip of a sterile Kalayjian culture instrument within its protective wrapper.
Asbury AC (1985)
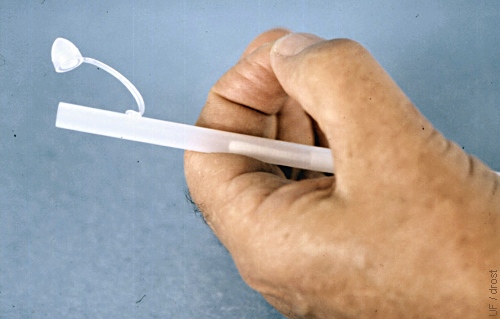
After Withdrawal of Kalayjian Culture Instrument.
Before withdrawal of the Kalayjian culture instrument from the uterine lumen the swab is retracted within the cannula. When the entire instrument is withdrawn the small, formerly protective, little cap is filled with uterine fluid.
Asbury AC (1985)
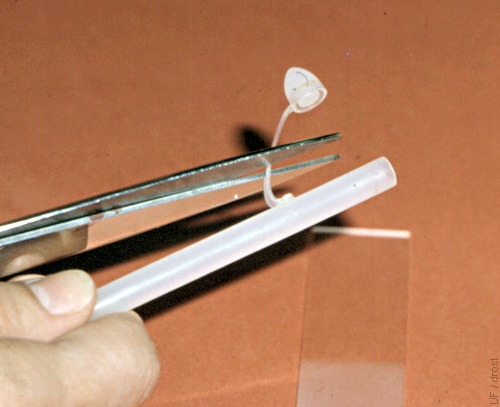
Removal of the Small Cap.
The small formerly protective cap is snipped off.
Asbury AC (1985)
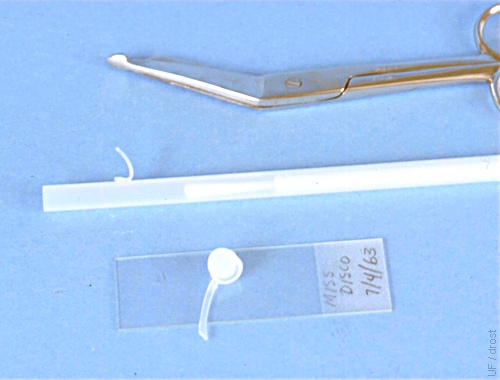
Small Cap Placed on Slide.
After the small cap has been snipped off it is placed upside down on a microscope slide to allow the contents to drain out.
Asbury AC (1963)
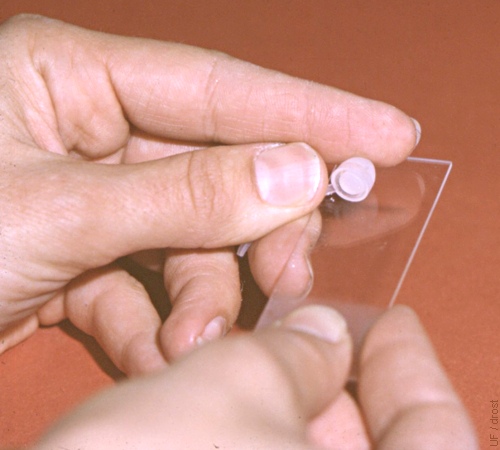
Drop of Uterine Fluid Poured onto Slide.
A drop of uterine fluid is transferred to a microscope slide.
Asbury AC (1985)
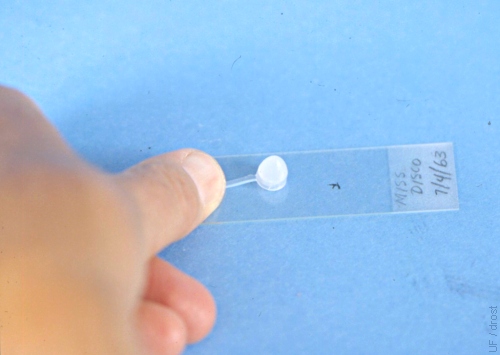
Uterine Fluid Placed on Slide.
The contents of the small cap are poured onto the microscope slide for cytological evaluation.
Asbury AC (1963)

Staining Solutions.
Dif-Quick staining solutions. From left to right, Fixative (methanol), Eosin, and Thizine. Uterine samples are held for 8 to 10 sec in each solution, semen samples for 30 sec, 1 minute, and 2 minutes respectively.
Asbury AC (1985)
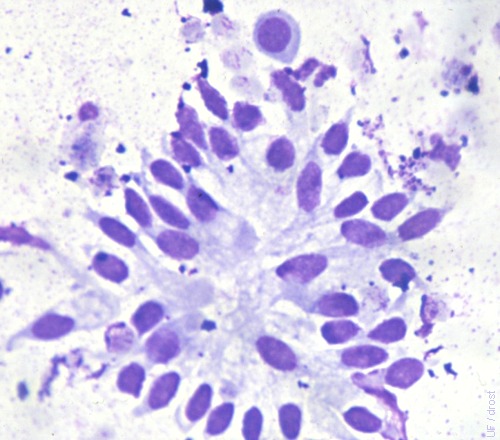
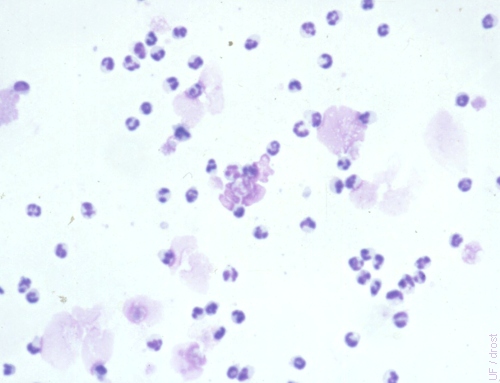
Raft of Epithelial Cells.
Stained endometrial smear of normal (= fewer than 5 neutrophils) glandular epithelial cells. Low power magnification (200 X).
Asbury AC (1985)
Neutrophils.
The finding of neutrophils indicates inflammation and is suggestive of endometritis. Low power view, 200 X.
Asbury AC (1985)
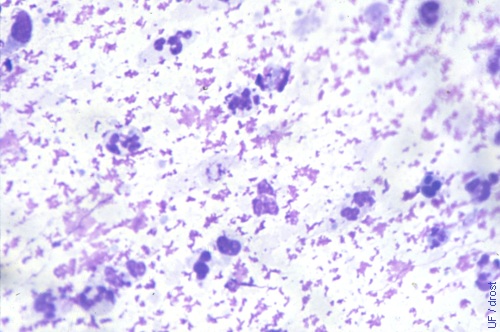
Close-up of Neutrophils.
The presence of neutrophils indicates inflammation and is suggestive of endometritis.
Asbury AC (1985)
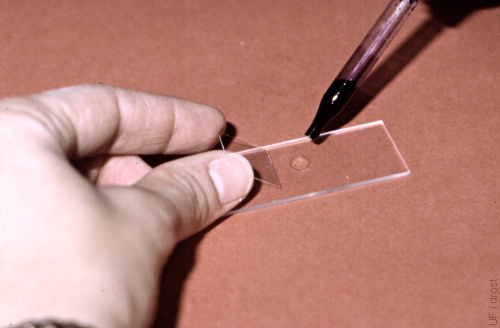
Methylene Blue is Added.
A drop of Methylene Blue stain is added to the drop of uterine fluid on the slide to identify yeast.
Asbury AC (1985)
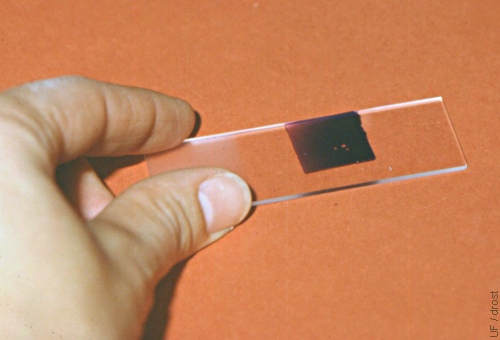
Placement of a Cover Slip.
After mixing the drops of uterine fluid and Methylene Blue stain, a cover slide is placed on the mixture. The slide is now ready for examination under the microscope at 200 X magnification for the presence of yeast.
Asbury AC (1985)
Sample Collection 1 A.
Method A. A sterile surgical glove is donned over a palpation sleeve. Sterile KY jelly is applied to the back of the fingers and hand.
Asbury AC (1978)

Sample Collection 2 A.
Method A. The sterile guarded culture instrument is laid on the sterile gloved hand which will cover it as it is passed through the vestibule and vagina.
Asbury AC (1978)

Sample Collection 3 A.
Method A. The sterile culture instrument, protected by the sterile gloved hand, is inserted into the external cervical os.
Asbury AC (1978)

Sample Collection 1 B.
Method B. Two new aseptic gloves are donned in preparation for the insertion of the sterile culture instrument into the vagina.
Asbury AC (1978)

Sample Collection 2 B.
Method B. The sterile guarded culture instrument is inserted between two aseptic palpation sleeves and is extended into the index finger of the outer glove, to enable insertion into the external os of the cervix.
Asbury AC (1978)

Sample Collection 3 B.
Method B. This image illustrates how the culture instrument penetrates the tip of the index finger of the glove, like when the finger is inserted in the cervix.
Asbury AC (1978)

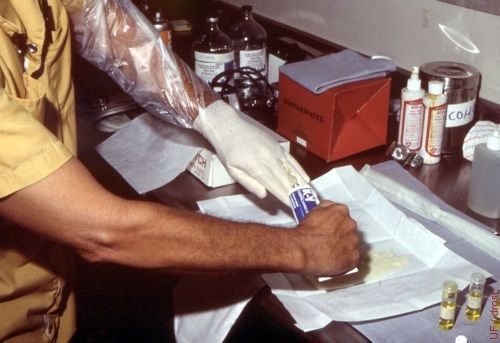
Streaking the Culture Plate.
The exposed culture swab is streaked onto the blood agar plate.
Asbury AC (1978)
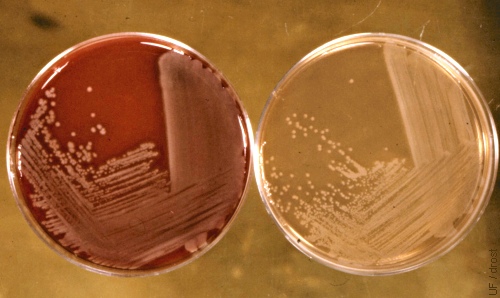
Pseudomonas Aeruginosa.
Growth of Pseudomonas aeruginosa on the red blood agar plate on the left, and on the clear MacConkey plate on the right.
Asbury AC (1978)
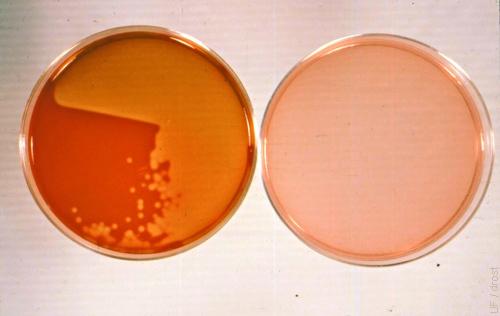
Bacillus Streptococcus.
Growth of Bacillus streptococcus on the blood agar plate on the left. No growth after streaking with the same swab on the MacConkey plate on the right.
Asbury AC (1978)
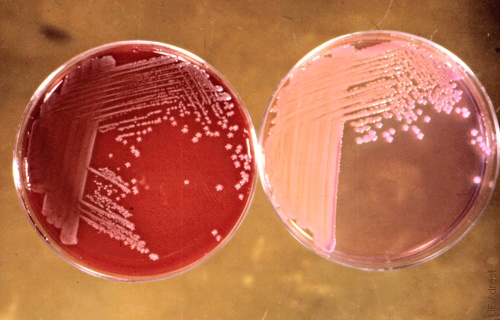
Klebsiella Pneumoniae.
Growth of Klebsiella pneumoniae on the blood agar plate on the left as well as on the MacConkey medium on the right.
Asbury AC (1978)

Uterine Biopsy Instrument.
Uterine biopsy instrument stored in a disinfectant solution. Autoclaving tends to dull the cutting edges.
Asbury AC (1977)
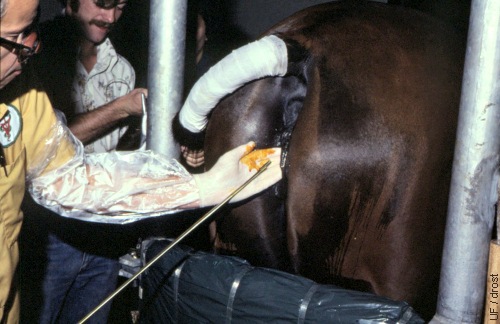
Introduction of the Biopsy Instrument.
The uterine biopsy instrument is passed into and through the cervix with digital guidance. Once the tip has entered the uterine body it is guided transrectally to the area of interest.
Asbury AC (1977)

Obtaining a Biopsy Specimen.
Once the tip of the biopsy instrument has entered the uterine body it is guided transrectally to the area of interest and a piece of endometrium is snipped off.
Asbury AC (1977)
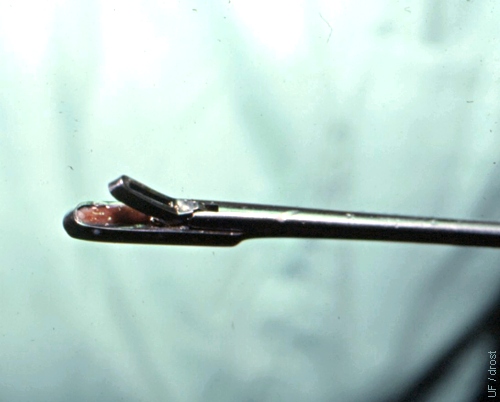
Specimen Obtained.
The tip of the biopsy instrument is shown with the endometrial specimen in the basket.
Asbury AC (1977)

Biopsy Site.
Uterine lumen exposed to show the site at which the biopsy specimen was taken 24 hours earlier.
Utrecht (1976)
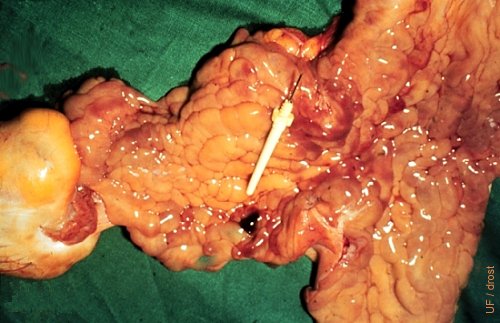
Biopsy Site - Close-up.
Uterine lumen exposed to show the site at which the biopsy specimen was taken 24 hours earlier. A small blood clot has formed.
Utrecht (1976)

Specimen Ready for Bouin's Solution.
The endometrial biopsy specimen is transferred to a vial of Bouin's fixative.
Asbury AC (1977)

Transfer to the Bouin's Solution.
The specimen is carefully dislodged from the basket of the biopsy instrument with a 25 ga needle, and placed in the fixative solution.
Asbury AC (1977)

Specimen Transferred Bouin's Solution.
The uterine biopsy specimen is gently lowered into the Bouin's fixative.
Asbury AC (1977)
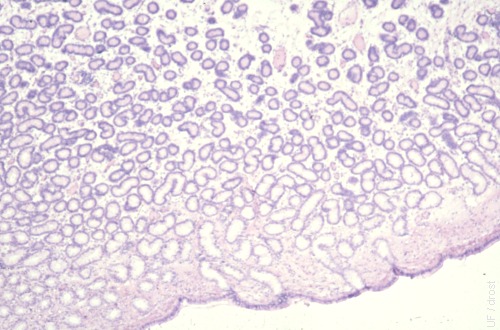
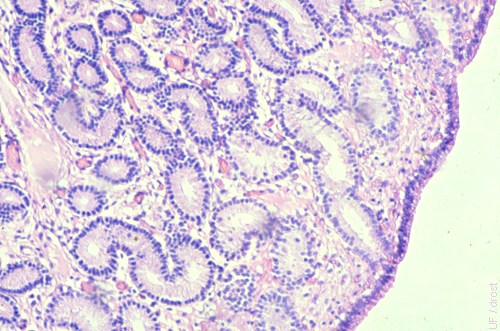
Normal Glandular Density.
Good glandular density. No glandular nesting. Low power magnification, 100 - 200 X.
Asbury AC (1981)
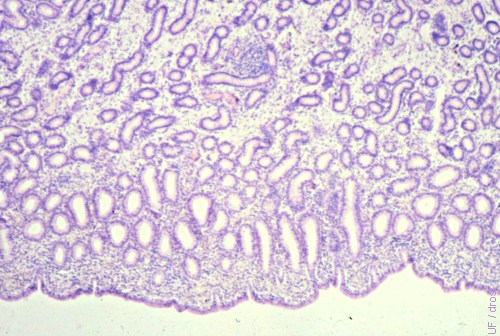
Good Glandular Density.
Normal glandular density with a few inflammatory cells in the stratum compactum. Magnification 400 X.
Asbury AC (1981)
Moderate Inflammation.
There is evidence of moderate inflammation by diffuse inflammatory cells below the epithelium. There is one inflammatory nidus in the center near the top.
Asbury AC (1981)
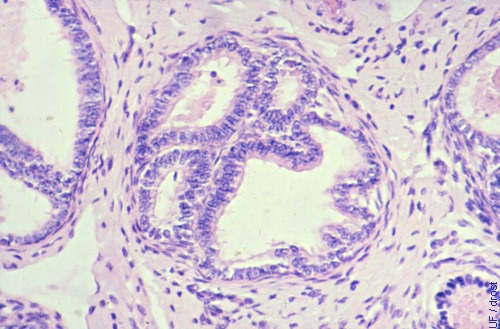
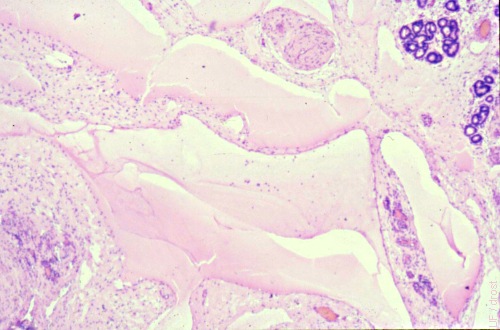
Periglandular Fibrosis.
Periglandular fibrosis (3 to 5 layers) with nesting and cystic glandular degeneration.
Asbury AC (1981)
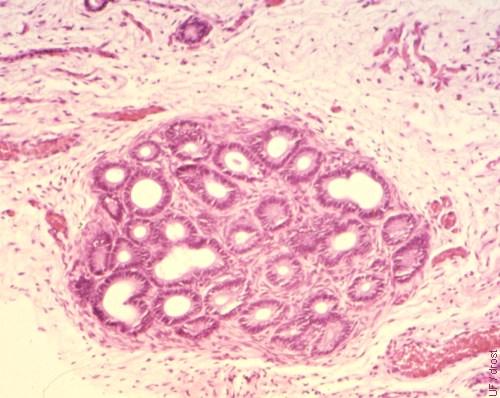
Cystic Glandular Degeneration.
Periglandular fibrosis with nesting and cystic glandular degeneration.
Asbury AC (1981)
Diffuse Inflammation.
Diffuse inflammation in the stratum compactum with transmigration of neutrophils through the endometrium. Magnification, 400 X.
Asbury AC (1981)
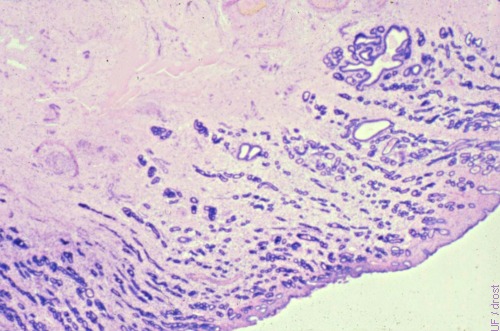
Lymphatic Lacunae.
Lymphatic lacunae in the stratum spongiosum. Glandular nesting in the upper right hand corner. Low power 200 X.
Asbury AC (1981)
Low Glandular Density.
Low glandular density with some cystic glandular degeneration. Low power, 200 X.
Asbury AC (1981)

Hematoma in the Broad Ligament.
This hematoma in the broad ligament was caused by rupture of the uterine artery in an aged Shetland pony mare. The mare went into shock and died.
Utrecht (1976)

Uterine Lavage Fluid.
Bucket full of lavage fluid for evaluation. Gross appearance is normal in this instance.
Pozor MA (2009)

Pyometra.
Pyometra in a mare with an occluded cervix due to adhesions. Both horns are distended with pus.
McEntee K (1972)

Pyometra.
Opened uterus of a mare with pyometra and an occluded cervix due to adhesions [the size of the square tile is 15 cm].
Roberts SJ (1972)
Mucometra.
A rare case of mucometra in the mare, caused by generalized cystic endometrial hyperplasia.
Roberts SJ (1972)

Cystic Endometrial Hyperplasia.
Cystic hyperplasia of the endometrium.
Roberts SJ (1973)

Endometrial Hyperplasia.
Cystic hyperplasia in a mare that has recently ovulated. The cysts are highlighted on pieces of white paper.
Roberts SJ (1972)

Uterine Lavage.
Older method of uterine lavage with a stomach tube and a funnel and gravity flow in a mare with pyometra and cervical adhesions. Currently a stomach tube and a stomach pump are more commonly used.
Pozor MA (2009)

Uterine Drainage.
Malodorous uterine fluids are drained from the uterus of a mare with pyometra.
Pozor MA (2009)
