
Vagina.
Vagina opened up dorsally. The cervix is on the left. Junction of the vagina and the vestibule is on the right.
Shille VM (1980)
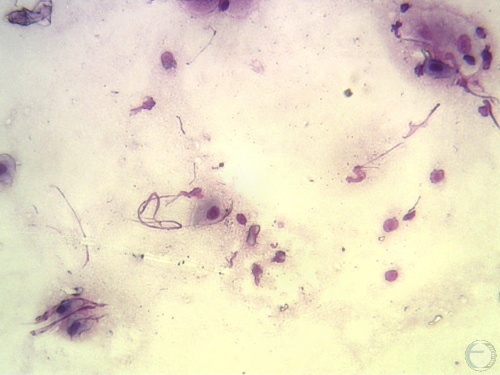
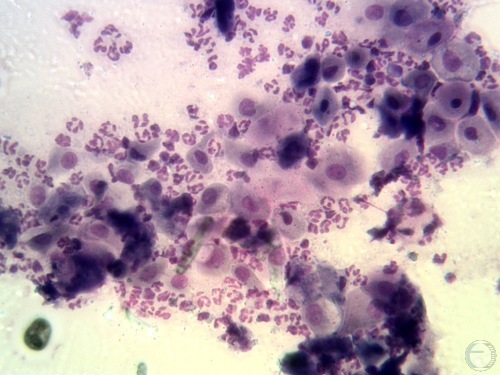
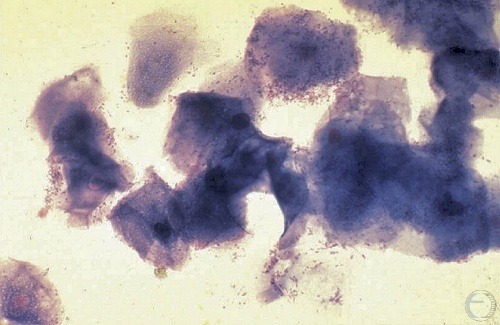
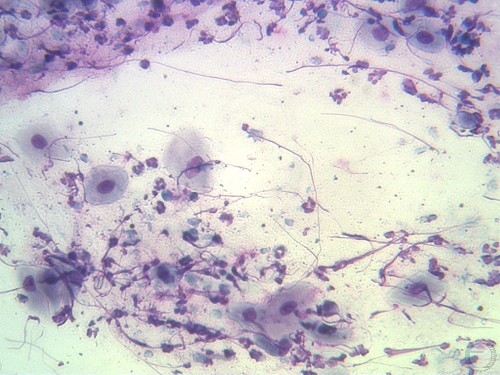
Vaginal Smear - Anestrus.
Vaginal cytology indicative of anestrus. Note the overall scant number of epithelial cells that tend to be misshapen parabasal or small intermediate cells. Some cells are broken and only the nuclei are visible with some cytoplasmic streaming. Note also the mucus and over all "dirty" background.
Verstegen J (2009)
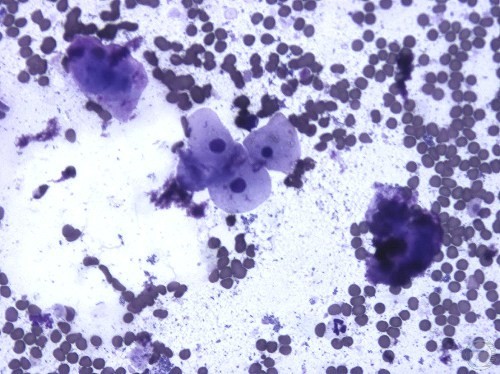
Vaginal Smear - Proestrus.
Vaginal cytology indicative of proestrus. Note the numerous red blood cells and occasional neutrophil. Epithelial cells are mostly intermediate with one superficial cell in this view.
Verstegen J (2009)
Vaginal Smear - Proestrus.
Vaginal cytology indicative of proestrus. Note the numerous red blood cells. No neutrophils are present in this view. Epithelial cells are mostly intermediate with one superficial cell in this view.
Verstegen J (2009)
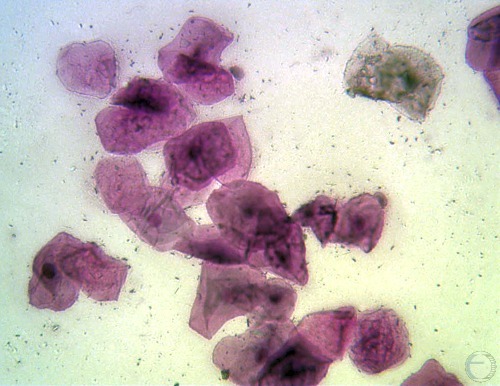
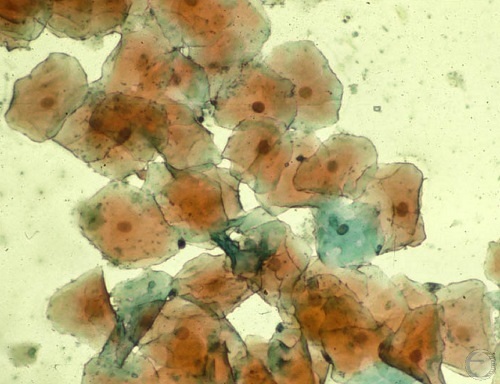
Vaginal Smear - Estrus.
Vaginal cytology indicative of estrus. Epithelial cells are superficial. Most are anuclear and some with fading or pyknotic nuclei. Note the absence of neutrophils (almost always true in estrus) and red blood cells (sometimes true in estrus), and the very clean background.
Verstegen J (2009)
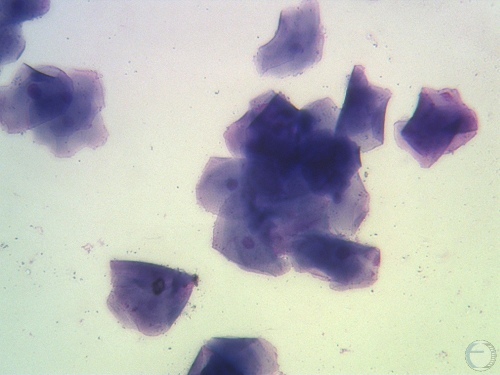
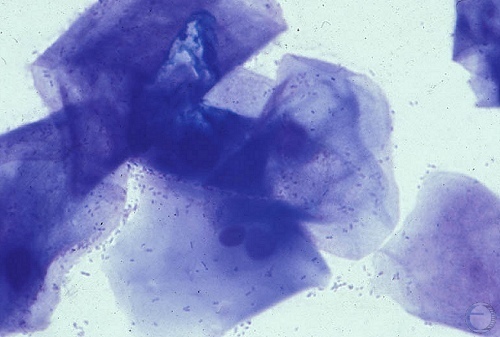
Vaginal Smear - Estrus.
Vaginal cytology indicative of estrus. Epithelial cells are superficial, most are anuclear, and some have fading or pyknotic nuclei. Note the absence of neutrophils (almost always true in estrus) and red blood cells (sometimes true in estrus). The background here is still relatively clean, but some bacteria are seen. This is not abnormal.
Verstegen J (2009)
Vaginal Smear - Mid-Estrus.
Vaginal cytology indicative of estrus. Epithelial cells are superficial. Most are anuclear and some with fading or pyknotic nuclei. Note the absence of neutrophils (almost always true in estrus) and red blood cells (sometimes true in estrus), and the very clean background.
Verstegen J (2009)
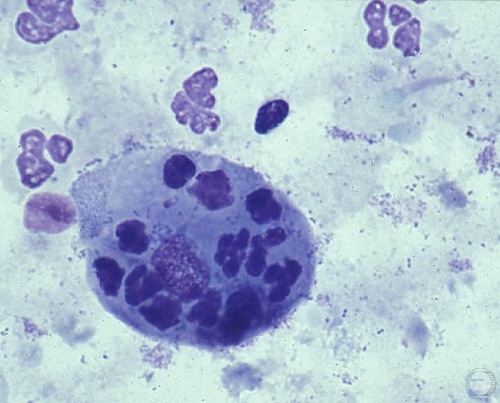
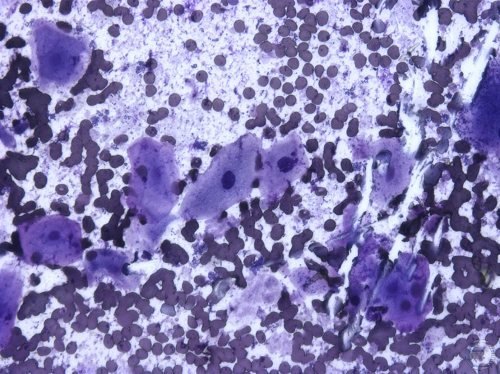
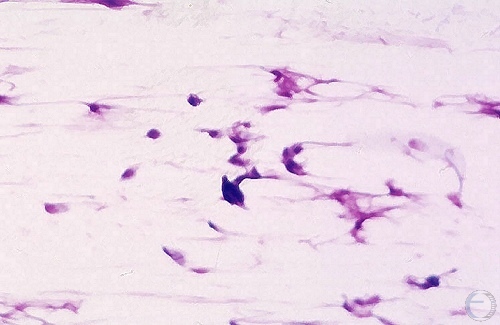
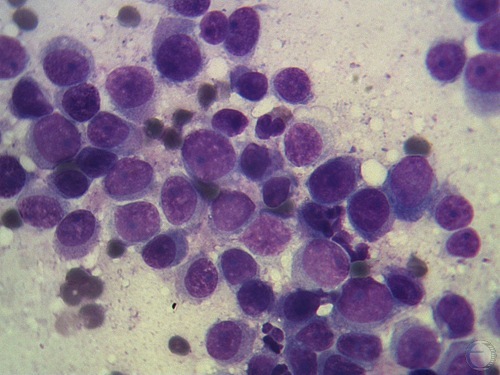
Vaginal Smear - Metestrus.
Vaginal cytology indicative of metestrus (early diestrus). Note the numerous neutrophils. A few neutrophils are located within the cytoplasm of intermediate epithelial cells. These cells are termed "metestral cells" and their presence is nearly pathognomonic for metestrus.
Verstegen J (2009)
Vaginal Smear - Metestrus.
Vaginal cytology indicative of metestrus (early diestrus). Note the numerous neutrophils. One or two neutrophils are located within the cytoplasm of intermediate epithelial cells. These cells are termed "metestral cells" and their presence is nearly pathognomonic for metestrus. The majority of epithelial cells are intermediate cells with a few parabasal and a few superficial cells.
Verstegen J (2009)
Vaginal Smear - Estrus.
Vaginal cytology indicative of estrus. Epithelial cells are superficial and most are anuclear. Some have fading or pyknotic nuclei. Note the absence of neutrophils (almost always true in estrus) and red blood cells (sometimes true in estrus). The background here is still relatively clean but some bacteria are seen. This is not abnormal.
Verstegen J (2009)
Vaginal Smear - Diestrus.
Vaginal cytology indicative of diestrus or anestrus. Epithelial cells are parabasal in nature. The presence of mucus is prevalent. Mucus tends to be absent during estrous cytology.
Verstegen J (2009)
Vaginal Smear - Metestrus.
Vaginal cytology indicative of metestrus (so long as the practitioner knew that the previous day's cytology was indicative of estrus). Numerous large intermediate cells are visible in this cytology. Even though neutrophils are not present the shift from anuclear superficial cells to large intermediate cells indicates the shift to metestrus.
Verstegen J (2009)
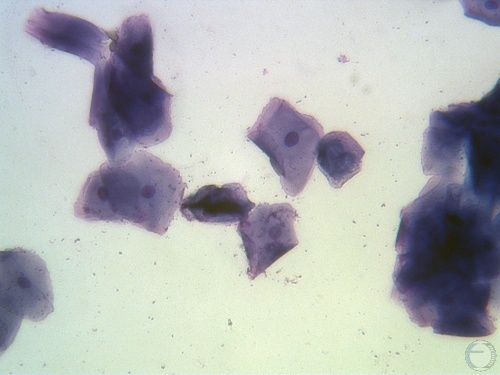
Vaginal Smear - Estrus.
Vaginal cytology indicative of estrus. Epithelial cells are superficial, most are anuclear, and some with fading or pyknotic nuclei. Note the absence of neutrophils (almost always true in estrus) and red blood cells (sometimes true in estrus), and the very clean background.
Verstegen J (2009)
Vaginal Smear - Metestrus.
Vaginal cytology indicative of metestrus (early diestrus). Note the numerous neutrophils. Metestral cells, per se, are not readily apparent in this view. Epithelial cells are intermediate cells. This smear could be confused with proestrus if it were not for the lack of red blood cells and the very numerous presence of neutrophils.
Verstegen J (2009)
Vaginal Smear - TVT.
Transmissible Venereal Tumor (TVT). Note the predominance of round cells. This sample can be easily obtained by rubbing the cauliflower-like tumor onto a glass slide.
Verstegen J (2009)

Prolapsed Vagina.
Considerable swelling and superficial trauma of the prolapsed vagina. The edema makes replacement more troublesome.
Hopper RM (2010)

Fresh Prolapsed Vagina.
Fresh, cleaned up, prolapsed vagina. Minimal trauma, good color.
LeBlanc MM (2013)

Fresh Prolapsed Vagina.
Lateral view of a fresh, cleaned up, prolapsed vagina. Minimal trauma, good color.
LeBlanc MM (2013)

Retention of a Prolapsed Vagina.
After replacement of the prolapsed vagina the mass is retained with horizontal mattress sutures placed laterally in the lips of the vulva. Small buttons are used to prevent the sharp suture material from cutting into the edematous labiae.
LeBlanc MM (2013)

Retention of a Prolapsed Vagina.
After replacement of the prolapsed vagina the mass is retained with horizontal mattress sutures placed laterally in the lips of the vulva. Small buttons are used to prevent the sharp suture material from cutting into the edematous labiae. Lateral view.
LeBlanc MM (2013)
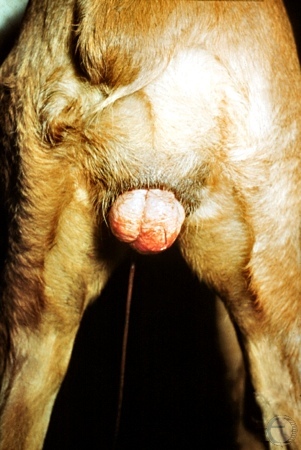
Chronic Prolapsed Vagina.
Chronic vaginal prolapse in an 11-month old dog.
Utrecht (1975)
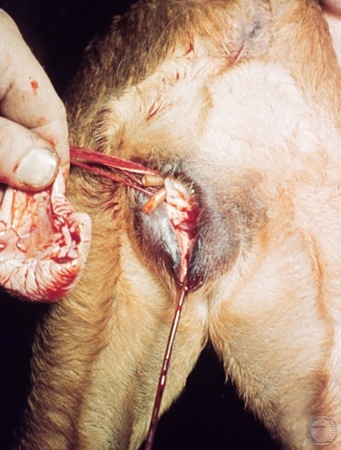
Prolapse Amputated.
The prolapsed portion of the vagina has been ligated and amputated.
Utrecht (1975)

Hyperplasia of Vaginal Floor 1.
Posterior view of a vaginal prolapse at time of initial presentation. The labiae are directed downwards.
Utrecht (1975)

Hyperplasia of Vaginal Floor 2.
Elevation of the prolapsed vagina by the perineum, at the time of presentation. The vaginal mucosa is visible. The labiae are swollen.
Utrecht (1975)

Hyperplasia of Vaginal Floor 3.
Gradual regression of the vaginal prolapse. Wrinkles appear in the skin five days after presentation. Labiae are still aimed downwards.
Utrecht (1975)

Hyperplasia of Vaginal Floor 4.
Further regression of the prolapsed mass ten days after presentation.
Utrecht (1975)

Hyperplasia of Vaginal Floor 5.
The vulvar cleft has returned to its approximately normal orientation by 22 days after presentation. The legs are soiled by a vaginal discharge. If the prolapse recurs amputation may be indicated.
Utrecht (1975)
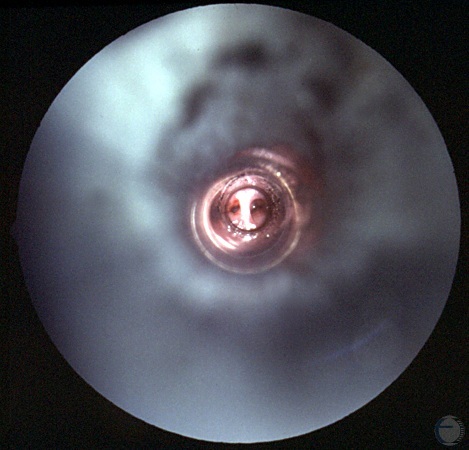
Vaginal Septum.
Vaginoscopic view of the anterior vagina. There is a dorsoventral septum.
Shille VM (1980)

